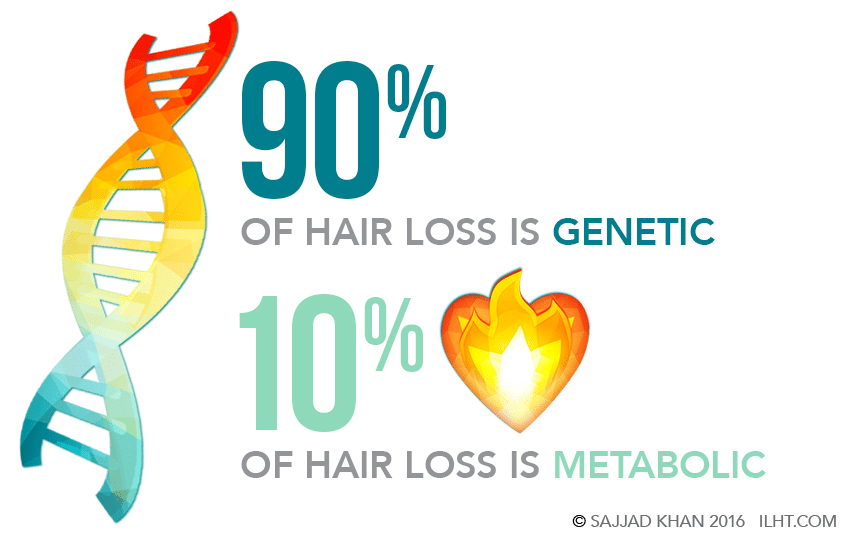
Half of all men will experience noticeable hair loss during their lifetime. The cause is genetic 90 percent of the time, while the rest is considered “metabolic” hair loss.
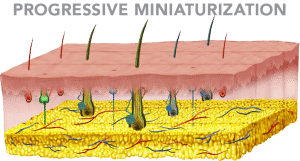
Hair loss genes passed down from either parent might activate at any time after maturity, depending on individual genetics. When activation occurs, hair becomes sensitized to di-hydro-testosterone, or DHT, a testosterone metabolite that kicks off a chain of events that leads to a pattern of progressive miniaturization of the hair follicle. Without treatment, these hair follicles eventually will die, leading to permanent hair loss.
If the hair loss genes activate earlier in life — for example, when a man is in his 20s — the rate of progressive miniaturization and hair loss will be highly accelerated when compared to activation that occurs when a man is older.
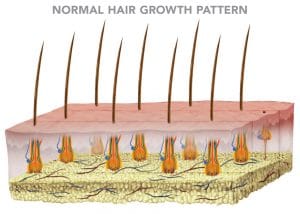
Normal Hair Growth
Hair is medically referred to as follicles. Each follicle grows as one, two or three hairs, or, more rarely, in groups of four or five hairs. Each follicular unit is equipped with its own glands, muscles, blood and nerve supplies.
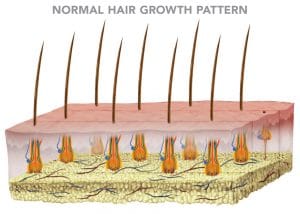
Each follicle has an average lifespan of three to seven years and grows approximately a half inch per month. This active period of growth is referred to as the anagen phase. When the anagen phase comes to an end, the hair enters a period of regression that lasts a few weeks called the catagen phase. After the catagen phase, the hair enters a resting period of an average three months called the telogen phase. When the telogen phase is over, the hair falls out and a new anagen growth phase begins with the hair growing back.
Under normal circumstances, 90 percent of our follicles are in the active anagen growth phase, while the remaining 10 percent are going through the catagen and telogen phases.
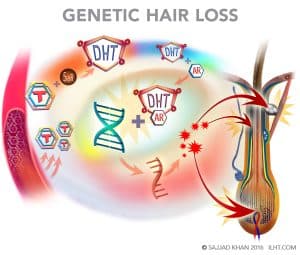
 Genetic Hair Loss and DHT
Genetic Hair Loss and DHT
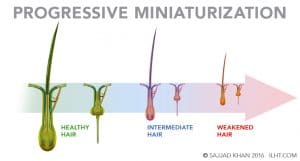
In genetic hair loss, testosterone primarily enters in the papilla, outer root sheath and sebaceous gland cells, where it is converted into Di-Hydro-Testosterone (DHT) by the enzyme 5-alpha reductase (5AR). The DHT binds to androgen receptors and enters the nucleus of these cells to bind with DNA, which in turn signals production of specific messenger RNA that creates follicle-damaging proteins, resulting in disruption to the normal hair-growth cycle. The anagen growth phase is cut short, and the hair regresses prematurely to the catagen phase and eventual resting telogen phase. Once the telogen phase is over, a new hair grows in but with a reduced diameter and an even shorter anagen growth phase.
This progressive miniaturization process repeats over and over with an ever-decreasing anagen growth phase and decreased hair diameter until eventually the hair is lost altogether.
Classification of Male Pattern Hair Loss
Genetic hair loss goes through typical sequences: Hair loss initially leads to gradual thinning and the frontal and temporal hairline starts receding. Finally, this develops into frontal baldness, later also involving the mid-scalp and crown area.
Male pattern hair loss is classified into seven types:
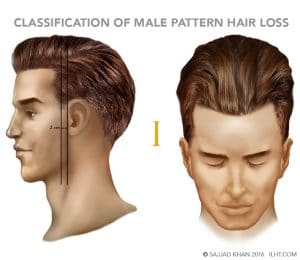
Type I
Minimal receding of the front hairline
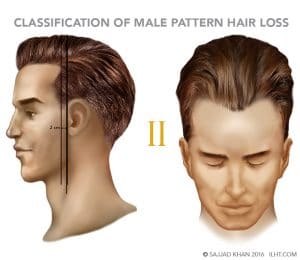
Type II
Receding of both the front and side hairlines; if a vertical line is drawn in front of the ear and a second vertical line is drawn 2 cm in front of the first, the triangular recession stops in front of the second vertical line
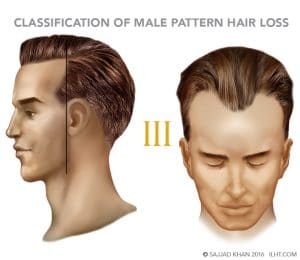
Type III
Receding of both the front and side hairlines, with the area of recession on both sides extending up to the vertical line in front of the ear
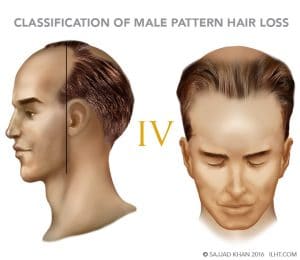
Type IV
The frontal and side hairlines have receded and become extremely thin, and the recession extends beyond the vertical line in front of the ear; established loss in the crown area, although it is still clearly separated from the frontal baldness by a band of hair
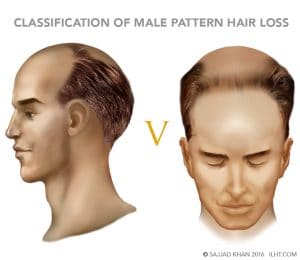
Type V
The front hairline is completely lost, but the front baldness and crown baldness are still separated from each other by a thin band of hair.
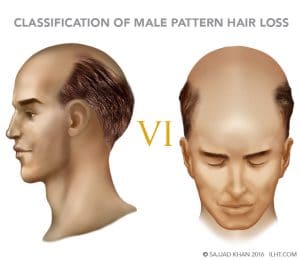
Type VI
The bridge between front and crown baldness is lost and the entire area of baldness is greater laterally and posteriorly than the Type 5 hair loss
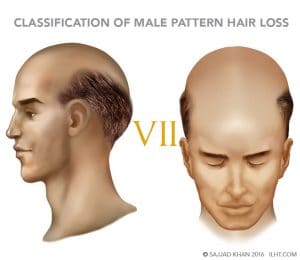
Type VII
The baldness is most severe; all that remains is a band of thin hair in the occipital, parietal and temporal area
Metabolic Hair Loss
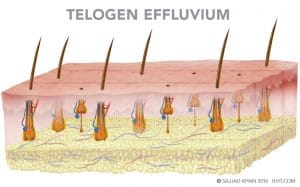
The process of metabolic hair loss is quite distinctive from genetic hair loss. There is no reduction in hair diameter or progressive miniaturization. With abrupt metabolic changes in the body, hair loss can start in few days, though it might start a few weeks or two to three months after the change. Normally 10 percent of the hairs on a scalp are in the resting telogen stage, but in metabolic hair loss, 20 to 50 percent of the follicles are in the telogen stage, leading to increased hair loss. Medically, the condition is called telogen effluvium.
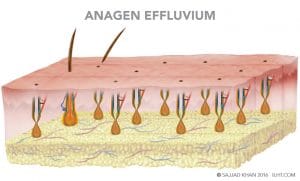
Occasionally in metabolic hair loss, more than 90 percent of the hair stops growing due to damage to the matrix cell in the area of the hair bulb. The shed hairs have a tapered down look like a pencil point; this hair loss is medically referred as anagen effluvium.
Metabolic conditions that can lead to hair loss:
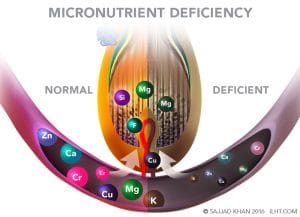
- Nutritional imbalance or deficiency
- Drastic weight loss

- Excessive stress

- Extreme illness
- Major surgery
- Medications, including beta blockers, antidepressants, non-steroidal anti-inflammatories and chemotherapy drugs

- Excessive intake of vitamin A
- Thyroid dysfunction

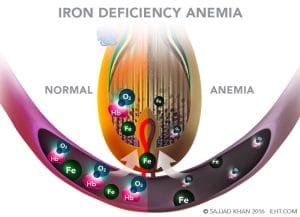
- Anemia
Metabolic hair loss is easy to treat, once its cause is identified. The good news is that metabolic hair loss is usually temporary in nature. When the stressful condition normalizes, the hair usually returns.
Diagnosis of Hair Loss
Although hair loss from metabolic causes happens only about 10 percent of the time, it’s important to rule out metabolic causes before attributing the hair loss to genetics.
The following methods of diagnosis are typically employed when identifying the root cause of hair loss:
- A detailed medical history of the client
- Densitometer examination of the hair and scalp condition
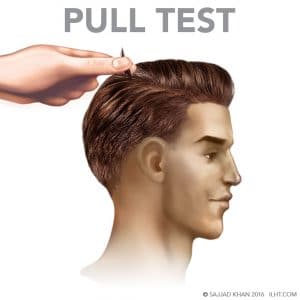
- Hair pull test
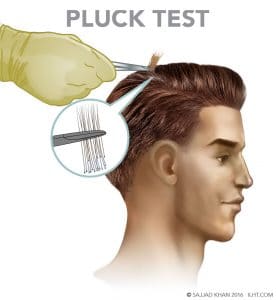
- Hair pluck test
- Evaluation of diagnostic lab test results
- Scalp biopsy
Detailed Medical History:
A complete medical history can provide extremely valuable information to pinpoint the cause of hair loss. The detailed history should focus on nutritional deficiencies, weight loss or gain, current medications, symptoms of hormonal changes, current stress situation, extreme sickness, recent major surgery and family history related to hair loss.
Densitometer Examination:
Hair density on the surface of the scalp can be evaluated using a densitometer, a high-power magnification device that provides information on hair density (spacing between follicular units), hair diameter and the degree of miniaturization that might be in progress. If
If spacing between follicular units is increased but without reduction in the hair diameter, this suggests metabolic hair loss. However, if the examination reveals 15 percent or more of the hair has reduced diameter, this is more suggestive of genetic hair loss.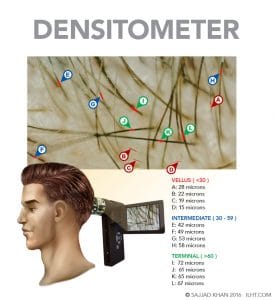
Hair-Pull Test:
This is a simple diagnostic test in which the physician lightly pulls on roughly 100 hairs to determine if an excessive loss is in progress. More than three hairs pulling from the scalp is considered abnormal.
Hair Pluck Test:
The medical professional plucks approximately 50 hairs from the client’s scalp and examines them under a microscope. Early hair loss can be diagnosed by comparing the percentage of anagen (growing) hair to telogen (resting) hair. Telogen hair has approximately half the follicle depth of anagen hair. If the ratio of telogen to anagen hair is 10 percent or less, early hair loss is not in progress. If the ratio rises to 15 percent, early hair loss is likely taking place, and if the ratio reaches 30 percent, active hair loss is taking place.
Diagnostic Lab Tests
Blood work can help pinpoint if hair loss is due to a metabolic condition linked to nutritional deficiency, anemia or hormonal imbalance.
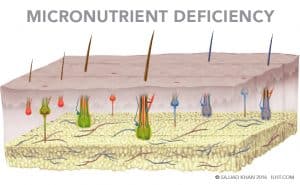
A micronutrient test is extremely helpful in providing detailed information if the patient has a deficiency in major minerals, trace minerals or vitamins critical to hair growth.
A complete blood and thyroid test will reveal if there are any abnormalities in serum iron, serum ferritin, total iron-binding capacity (TIBC) and thyroid hormones
Scalp Biopsy
A scalp biopsy involves a medical professional removing a very small section of the scalp (usually 4mm in diameter) and examining it under a microscope.
If an abnormally large percentage of telogen hair is found compared to anagen hair (telogen hair depth is approximately 50 percent of anagen), but no decrease is seen in the average hair diameter, the loss is likely due to telogen effluvium, a metabolic condition.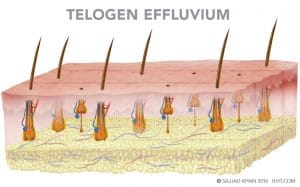
If the follicles have mostly normal depth but have tapering just above the papilla, the hair loss is most likely anagen effluvium, a metabolic condition usually associated with chemotherapy, although it also could be a patchy hair loss condition called alopecia areata. 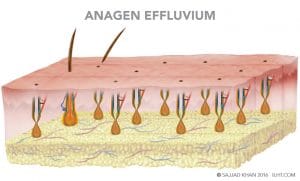
If there is no change in hair diameter but there is an overall reduction of the number of hairs within multi-follicular units, the likely reason is metabolic hair loss.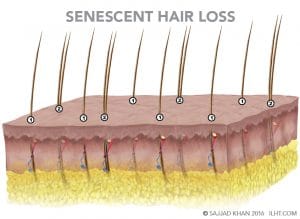
If hairs are found with varying depths and diameters, the most likely diagnosis would be genetic hair loss.
MEN’S HAIR LOSS TREATMENTS
Genetic hair loss treatments are generally one of two types: medical or surgical.
Medical treatments generally are one of three classes:
- Topical Minoxidil
- Oral Anti-Androgen Finasteride
- Regenerative Treatments – ECM, PRP, and LLLT
Minoxidil
Minoxidil, a vasodilator, is FDA approved to treat hair loss. Testing showed that a 5% solution or foam applied to the scalp twice a day resulted in an increase in hair regrowth in 45 percent of the male subjects.
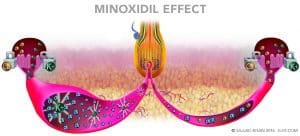 Side effects could include a skin rash, increase in heart rate, dizziness, and swelling.
Side effects could include a skin rash, increase in heart rate, dizziness, and swelling.
Finasteride
Finasteride, taken as a 1 mg daily tablet, reduces the production of DHT and DHT-induced hair damage. Finasteride can reverse the miniaturization process, reducing the hair loss. The thin, weakened hair can revert to healthy, normal hair, especially in the crown area. Finasteride is FDA approved for hair loss.
 Side effects include loss of libido or erectile dysfunction, which is reported by 0.3% of the younger individuals who take it, increasing to 3 to 5% of men 50 or older. Most of the time these side effects will disappear once the finasteride is stopped.
Side effects include loss of libido or erectile dysfunction, which is reported by 0.3% of the younger individuals who take it, increasing to 3 to 5% of men 50 or older. Most of the time these side effects will disappear once the finasteride is stopped.
In a few individuals, finasteride side effects can persist even after discontinuation of the medicine. These side effects are loss of libido, erectile dysfunction, depression, suicidal ideation, anxiety, panic attacks, gynecomastia, muscle atrophy, cognitive impairment, insomnia, severely dry skin and tinnitus. At the first sign of any of the above side effects, discontinue the finasteride immediately and consult with your doctor.
Extra Cellular Matrix (ECM)
Extra Cellular Matrix (ECM), injected into the scalp, forms a structural scaffolding and signals the bone marrow stem cells to move to the scaffold area. The scaffold act as a glue that holds the stem cells in the scalp and helps them start to work regenerating the follicles and new blood vessels, collagen, fat cells and skin cells. The process may help the weaker hair cells become stronger and restore the normal hair growth cycle.
 Platelet Rich Plasma (PRP)
Platelet Rich Plasma (PRP)
Platelet Rich Plasma (PRP) is prepared by putting a patient’s own blood in a centrifuge to concentrate and isolate the platelets and plasma from other blood cells. The concentrated platelets are activated, and they release growth factors. The fibrinogen in the plasma is also activated to provide the scaffold for growth factors to work and help the dormant papilla regenerate the hair. Platelet growth factors may reverse the miniaturization process and restore the normal hair cycle.
ECM and PRP can be injected into the scalp together; they complement each other in helping the weaker hair become stronger.
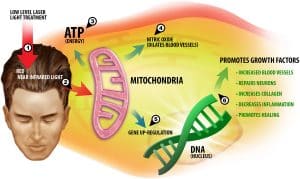
 Low Level Light Therapy (LLLT)
Low Level Light Therapy (LLLT)
Low Level Light Therapy (LLLT) applies a lower dose of near infrared light to promote tissue regeneration and reduce inflammation. The existence of nearly all life on Earth is fueled by light from the sun; the sunlight spectrum ranges mainly from ultraviolet to visible and infrared light. LLLT is in the near infrared spectrum, from 600 to 1000 nanometers. Typically, it is applied for a few minutes on alternate days. LLLT may reverse the hair thinning and restore the normal hair growth cycle.
 Surgical Treatments
Surgical Treatments
Surgical treatments for hair loss include different types of hair transplant procedures. Hair transplant is the only proven way to restore hair permanently onto the bald or thinning areas of the scalp.
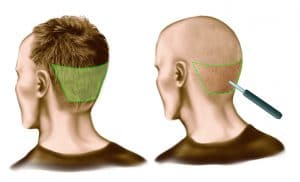
Under local anesthesia, hair is relocated from the back of the scalp to the thinning or bald areas. Because the transplanted hairs are genetically different from the ones that were lost, they are resistant to hair loss and will continue to grow permanently.
Natural and permanent results of hair transplantation demand clinical expertise and as well as artistic creativity and ability on the part of the surgeon.
Surgeons generally use one of the two standardized hair restoration techniques or a new technique still being perfected:
- Follicular Unit Extractions (FUE), in which follicular units are individually punched out from the back of the scalp and relocated to a thinning or bald area.
- Follicular Units Transplant (FUT), in which hair-bearing tissue is taken from the back of the scalp, individual follicular units are separated out from the tissue under microscopes, and the follicular units are transplanted into the thinning or bald area.
The technique of hair restoration surgery used on a particular client depends on his specific individual needs and lifestyle.
FUE
If the client prefers to wear his hair very short (#1 Clipper size, or about 1/8 of an inch long) or even shaved, FUE is the better choice because it does not leave any visible scarring in the donor area.
FUE requires the donor area be shaved for surgery, either partially or completely. If the donor area is completely shaved, an average of 2,000 to 3,000 follicular units can be extracted. If donor area is partially shaved so that the top hair will cover the shaved areas, an average of 1,000 to 1,500 follicular units can be extracted.
Special micro punches are used to remove the follicular units manually, motorized or robotically. The goal is to have minimum damage during FUE.
- Once the donor area heals, there is no noticeable scarring in the donor area.
- The client has the flexibility to wear the hair extremely short or even shaved without the fear of visible scarring
Disadvantages Of FUE:
- An average 5% of the follicular units extracted are damaged.
- Because the number of follicular units extracted in one surgery averages only 2,000 to 3,000, multiple hair transplants might be needed for optimal results.
- The surgery is noticeable for an average of 10 to 15 days.
- The patient experiences temporary numbness in the donor and transplanted area.
- The client could see shock hair loss in the transplanted area (although hair lost due to shock grows back along the transplanted hair).
FUT/Long Hair Technique
If the client would like to resume his usual routine the day following the surgery without it being noticeable, FUT is a good choice.
In FUT, an incision an average 0.5 mm deep is made at the upper and lower borders of the marked donor area. To extract the donor tissue, the incision margins are separated by special skin hooks without any further incision to avoid damage to the hair. The follicular units are then separated from the extracted tissue under microscopes.
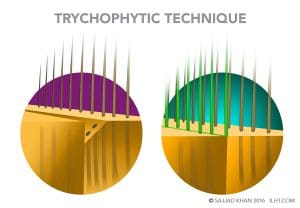
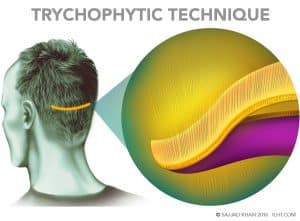 Removing that donor tissue leaves a 1 to 2 cm gap in the donor area, which is where the scarring can take place. However, the surgeon can reduce scarring by using the Trichophytic technique. The surgeon lays ECM in the tissue gap to promote healing, then shaves one edge of the gap and overlaps the edges to be fine-stitched together. As the incision heals, the hair will grow out through the fine scar line, which can make the scar undetectable even in short hair.
Removing that donor tissue leaves a 1 to 2 cm gap in the donor area, which is where the scarring can take place. However, the surgeon can reduce scarring by using the Trichophytic technique. The surgeon lays ECM in the tissue gap to promote healing, then shaves one edge of the gap and overlaps the edges to be fine-stitched together. As the incision heals, the hair will grow out through the fine scar line, which can make the scar undetectable even in short hair.
 Advantages of FUT/Long Hair Technique:
Advantages of FUT/Long Hair Technique:
- Damage to less than 0.5 percent of follicular units during preparation for transplant, compared to as much as 5 percent in the FUE procedure.
- An average 5,000 follicular units can be transplanted in one surgery, with a possibility of 7,000 to 8,000 if the flexibility and density is good.
- Higher follicular unit numbers transplanted and nearly 100% survival can help achieve the client’s goals in only one surgery.
- Long hairs transplanted in the hairline gives a good preview of the future hairline and outcome.
- Follicular units can be readjusted during the surgery if needed, depending on the initial look.
- There is no surgical downtime; the client could resume work the day after the procedure without it being noticeable.
Disadvantages of the Long Hair Technique:
- If a client later shaves the hair or has it cut extremely short, stitches marks or a fine line scar in the donor area could be noticeable.
- The patient experiences temporary numbness in the donor and transplanted area.
- The client could see shock hair loss in the transplanted area (although hair lost due to shock grows back along the transplanted hair).
Reasons to Choose FUT
- If the client wears his hair a half an inch or more in length most of the time, the long hair technique is the absolute best choice.
- There is no surgical downtime; the individual can resume the work very next day.