Approximately 40 percent of women will experience hair loss during their lifetime. The cause is genetic about half the time, while the other half of the time it is considered “metabolic” in nature.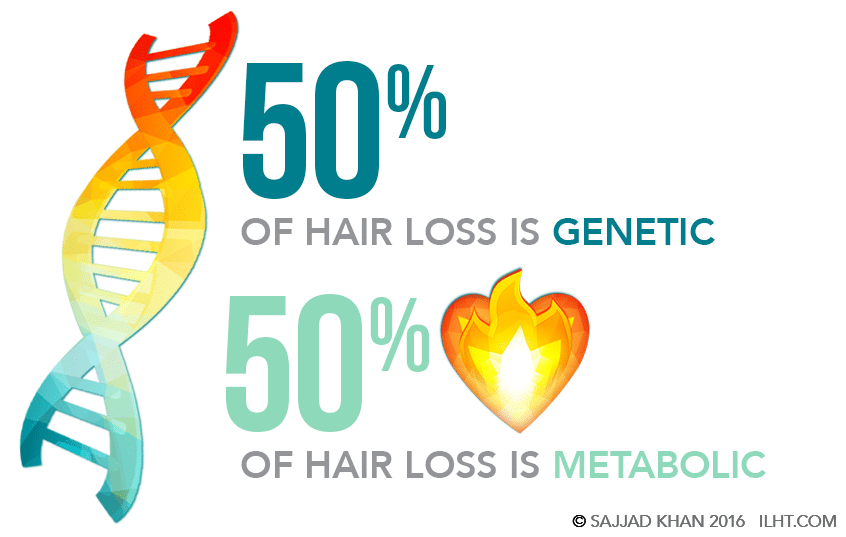 Genetic hair loss usually starts as a progressive reduction of the hair diameter. Without treatment, the weakened hairs will fall out and result in permanent loss.
Genetic hair loss usually starts as a progressive reduction of the hair diameter. Without treatment, the weakened hairs will fall out and result in permanent loss.
Hair loss genes passed down from either parent might activate at any time after maturity, depending on individual genetics. When activation occurs, hair becomes sensitized to di-hydro-testosterone, or DHT, a testosterone metabolite that kicks off a chain of events that leads to a pattern of progressive miniaturization of the hair follicle. Without treatment, these hair follicles eventually will die, leading to permanent hair loss.
If the hair loss genes activate earlier in life — for example, when a woman is in her 20s — the rate of progressive miniaturization and hair loss will be highly accelerated when compared to activation that occurs when she is older.
Metabolic hair loss, on the other hand, is usually attributed to abrupt changes in the body –such as an illness, sudden weight loss or medication change – and most often is temporary.
Normal Hair Growth
Hair is medically referred to as follicles. Each follicle grows as one, two or three hairs, or, more rarely, in groups of four or five hairs (called “follicular units.”) Each follicular unit is equipped with its own glands, muscles, blood and nerve supplies.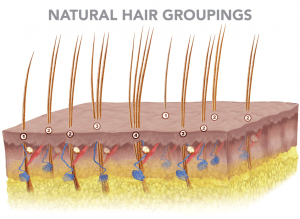 Each follicle has an average lifespan of three to seven years and grows approximately a half inch per month. This active period of growth is referred to as the anagen phase. When the anagen phase comes to an end, the hair enters a period of regression that lasts a few weeks called the catagen phase. After the catagen phase, the hair enters a resting period of an average three months called the telogen phase. When the telogen phase is over, the hair falls out and a new anagen growth phase begins with the hair growing back.
Each follicle has an average lifespan of three to seven years and grows approximately a half inch per month. This active period of growth is referred to as the anagen phase. When the anagen phase comes to an end, the hair enters a period of regression that lasts a few weeks called the catagen phase. After the catagen phase, the hair enters a resting period of an average three months called the telogen phase. When the telogen phase is over, the hair falls out and a new anagen growth phase begins with the hair growing back.
Under normal circumstances, 90 percent of follicles are in the active anagen growth phase, while the remaining 10 percent are going through the catagen and telogen phases.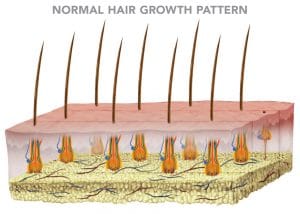
Genetic Hair Loss and DHT
In genetic hair loss, testosterone enters in the papilla, outer root sheath and sebaceous gland cells, where it is converted into DHT by the enzyme 5-alpha reductase (5AR). The DHT binds to androgen receptors and enters the nucleus of these cells to bind with DNA, which in turn signals the production of specific messenger RNA that creates follicle-damaging proteins, resulting in disruption to the normal hair-growth cycle. The anagen growth phase is cut short, and the hair regresses prematurely to the catagen phase and eventual resting telogen phase. Once the telogen phase is over, a new hair grows in but with a reduced diameter and an even shorter anagen growth phase. This progressive miniaturization process repeats over and over with an ever-decreasing anagen growth phase and decreased hair diameter until eventually the hair is lost altogether.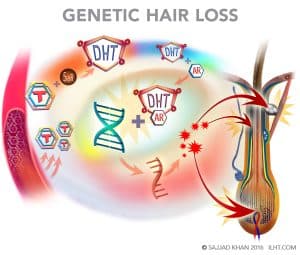
Women who develop female-pattern hair loss have a relatively increased amount of 5AR and androgen receptors in the frontal and mid-scalp areas. Most women with genetic hair loss have diffuse thinning and a milder expression of hair loss at the hairline when compared to men with male-pattern balding because women have 50 percent less 5AR and androgen receptors and six times more enzyme aromatase than men. The aromatase converts the testosterone to estrogen, so less testosterone is available to get converted into DHT in hair cells.
Genetic or female pattern hair loss can start at any age, but once it starts it continues for the rest of the life. It begins with a general thinning behind the hairline in the frontal and mid-scalp areas. Initially, the hairline is not affected, but as the hair loss continues, the crown area and hairline are both affected as well.
Genetic hair loss can be triggered and accelerated by androgen-producing polycystic ovarian syndrome, or by taking high-androgen-index birth control pills, as well as during menopause when female hormone levels drop, giving an edge to androgens.
Classification of Female Pattern Hair Loss:
In 1977, Ludwig classified genetic hair loss into three stages: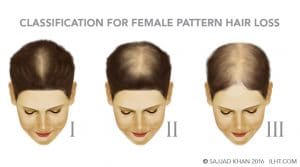
Stage I:
General thinning in the frontal, mid-scalp and crown regions. The frontal and temporal hairlines remain dense.
Stage II:
More pronounced thinning in the frontal, mid-scalp and crown regions. In addition, the frontal and temporal hairline starts thinning as well.
Stage III:
Extensive thinning in the frontal, mid-scalp and crown regions, with the frontal and temporal hairlines becoming very thin.
Later, Olsen described female genetic hair loss as a gradual increase in diffuse hair loss toward the front of the scalp in a “Christmas Tree” pattern.
Metabolic Hair Loss
The process of metabolic hair loss is quite distinctive from genetic hair loss. There is no reduction in hair diameter or progressive miniaturization. With abrupt metabolic changes in the body, hair loss can start in few days, though it might start a few weeks or two to three months after the change. Normally 10 percent of the hairs on a scalp are in the resting telogen stage, but in metabolic hair loss, 20 to 50 percent of the follicles are in the telogen stage, leading to increased hair loss. Medically, the condition is called telogen effluvium.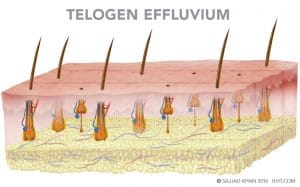
Occasionally in metabolic hair loss, more than 90 percent of the hair stops growing due to damage to the matrix cell in area of the hair bulb. The shed hairs have a tapered down look like a pencil point; this hair loss is medically referred as anagen effluvium.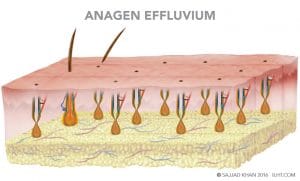
Metabolic hair loss is easy to treat, once its cause is identified. The good news is that metabolic hair loss usually is temporary in nature. When the stressful condition normalizes, the hair usually returns.
Metabolic conditions that can lead to hair loss:
- Nutritional imbalance or deficiency
- Extreme dieting
- Excessive intake of vitamin A
- Traction alopecia, caused by tightly pulled hairstyles or the use of hair extensions
- Excessive stress
- Pregnancy
- Menopause
- Extreme illness
- Major surgery
- Shock
- Anemia
- Medications, including contraceptives, antidepressants, beta blockers, non-steroidal anti-inflammatories and chemotherapy drugs
- Polycystic ovarian syndrome
- Hormonal imbalances
- Thyroid dysfunction
Iron Deficiency Anemia is very common, especially in women, and is one of the major causes of temporary hair loss in women. Iron is very important in maintaining many body functions, including the production of hemoglobin, the molecule in your bloodstream that carries oxygen. Iron is also necessary for maintaining healthy skin, hair and nails.
Symptoms of iron-deficiency anemia are related to decreased oxygen delivery to the body and may include:
- Unusual paleness
- Unexplained fatigue or lack of energy
- Rapid heartbeat
- Brittle nails
- Hair loss
Oral and injectable hormonal contraceptives may trigger hair loss in women, especially if a genetic predisposition for hair loss already exists. Hair loss is often associated with a use of certain other prescription medicines, including beta blockers, antidepressants, non-steroidal anti-inflammatories and chemotherapy drugs.
Hypothyroidism (underactive thyroid) is a condition affecting the small butterfly-shaped thyroid gland at the base of the neck just below the Adam’s apple. Hormones that are produced by the thyroid gland — such as triiodothyronine (T3) and thyroxine (T4) — have an enormous impact on health by affecting all aspects of cellular metabolism. They control the rate which the body uses fats and carbohydrates, help control body temperature, influence heart rate and help regulate production of proteins in the body.
Symptoms of Hypothyroidism:
- Fatigue
- Weakness
- Weight gain or increased difficulty losing weight
- Coarse, dry hair
- Hair loss
- Dry and rough skin
- Paleness
- Cold intolerance
- Frequent muscle cramping and aches
- Constipation
- Depression
- Irritability
- Memory loss
- Abnormal menstruation
- Decreased libido
Hyperthyroidism (overactive thyroid) is a condition in which the thyroid gland produces too much of the hormone thyroxine.
Symptoms of hyperthyroidism:
- Sudden weight loss, even when the appetite or amount and type of food eaten remain the same or increase
- Rapid heartbeat (tachycardia) of more than 100 beats a minute
- Irregular heartbeat (arrhythmia)
- Hard pounding of the heart (palpitations)
- Increased appetite
- Nervousness, anxiety and irritability
- Tremors, usually fine trembling in hands and fingers
- Sweating
- Changes in menstrual patterns
- Increased sensitivity to heat
- Changes in bowel patterns, especially more frequent bowel movements
- An enlarged thyroid gland (goiter), which may appear as a swelling at the base of the neck
- Fatigue and muscle weakness
- Difficulty sleeping
- Skin thinning
- Fine and brittle hair
- Hair loss
Polycystic ovarian syndrome (PCOS) is a common endocrine system disorder among women of reproductive age. Women with PCOS may have enlarged ovaries that contain small collections of fluid in the follicles, as seen during an ultrasound exam.
PCOS is thought to be caused by excess androgen (male hormone). Not only is the male hormone elevated, but some of the excess androgen hormones are converted to estrogen, resulting in hormonal imbalance that can manifest itself by infrequent or prolonged menstrual periods, excess body hair (hirsutism), adult acne or severe adolescent acne, hair loss and obesity.
Menopause is the end of a woman’s menstrual cycle, defined as 12 consecutive months without a period. Menopause usually occurs in a woman’s 40s or 50s, with the average age around 50.
Menopause symptoms
- Hot flashes
- Night sweats
- Sleep problems
- Mood changes
- Weight gain due to slowing metabolism
- Thinning hair
- Dry skin
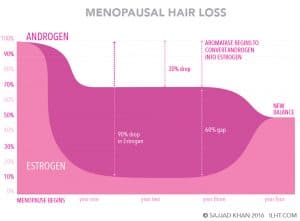
In menopause women have a 90 percent drop in estrogen with a 30 percent drop in androgens, leading to a relative androgen excess. This relative androgen excess not only can cause hair loss but it also increases the risk of heart disease during this period.
Three to four years after menopause, some of these androgens can be converted to estrogen, striking a new balance between estrogens and androgens.
Hair Loss Diagnosis:
The following methods are typically employed in diagnosing the root cause of hair loss:
- A detailed medical history
- Densitometer examination of the scalp hair and scalp condition
- Hair pull test
- Hair pluck test
- Evaluation of the diagnostic lab test results
- Micronutrient test
- Complete blood test
- Hormonal test
- Scalp biopsy
Detailed Medical History:
A complete medical history can provide extremely valuable information to pinpoint the cause of hair loss. The detailed history should focus on nutritional deficiencies, weight loss or gain, current medications, symptoms of hormonal changes, current stress situation, extreme sickness, recent major surgery and family history related to hair loss.
Densitometer Examination
Hair density on the surface of the scalp can be evaluated using a densitometer, a high-power magnification device that provides information on hair density (spacing between follicular units), hair diameter and the degree of miniaturization that might be in progress.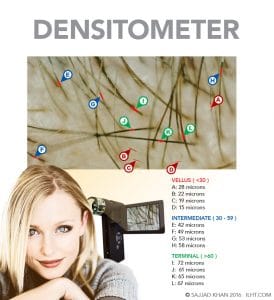
If spacing between follicular units is increased but without reduction in the hair diameter, this suggests metabolic hair loss. However, if the examination reveals 15 percent or more of the hair has reduced diameter, this is more suggestive of genetic hair loss.
Hair-Pull Test
This is a simple diagnostic test in which the physician lightly pulls on roughly 100 hairs to determine if an excessive loss is in progress. More than four hairs pulling from the scalp is considered abnormal.

Hair Pluck Test
The medical professional plucks approximately 50 hairs from the client’s scalp and examines them under a microscope. Early hair loss can be diagnosed by comparing the percentage of anagen (growing) hair to telogen (resting) hair. Telogen hair has approximately half the follicle depth of anagen hair. If the ratio of telogen to anagen hair is 10 percent or less, early hair loss is not in prpogress. If the ration rises to 15 percent, early hair loss is likely taking place, and if the ratio reaches 30 percent, active hair loss is taking place.
Diagnostic Lab Tests
Blood work can help pinpoint if hair loss is due to a metabolic condition linked to nutritional deficiency, anemia or hormonal imbalance.
A micronutrient test is extremely helpful in providing detailed information if the patient has a deficiency in major minerals, trace minerals or vitamins critical to hair growth.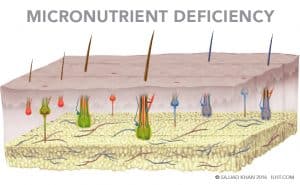
A complete blood count is performed to analyze hemoglobin, serum iron, serum ferritin, and total iron binding capacity (TIBC) to diagnose anemia.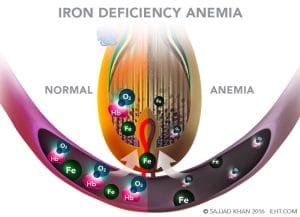
In addition, a complete hormonal analysis is performed measuring levels of DHEA, testosterone, androstenedione, prolactin, follicular stimulating hormone, luteinizing hormone and thyroid hormone. If any of these are not in the normal range, they could trigger or contribute to hair loss.
Scalp Biopsy
A scalp biopsy involves a medical professional removing a very small section of the scalp (usually 4mm in diameter) and examining it under a microscope to determine the cause of hair loss. If an abnormally large percentage of telogen hair is found compared to anagen hair (telogen hair depth is approximately 50 percent of anagen), but no decrease is seen in the average hair diameter, the loss is likely due to telogen effluvium, a metabolic condition.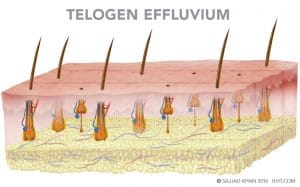
If the follicles have mostly normal depth but have tapering just above the papilla, the hair loss is most likely anagen effluvium, a metabolic condition usually associated with chemotherapy.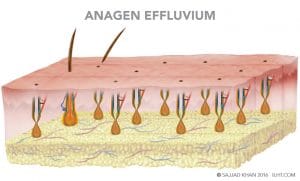
If hairs have varying depths and diamaters, the most likely diagnosis would be genetic hair loss.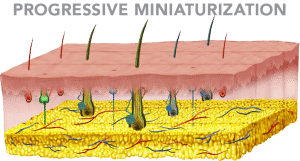
WOMEN’S HAIR LOSS TREATMENTS
This article contains a lengthy explanation of the subject and is divided into two parts for easy reading. Please choose the subject that matters to you the most by clicking on the following links
TREATMENTS FOR GENETIC HAIR LOSS IN WOMEN
Genetic hair loss treatments are generally one of two types: medical or surgical.
Medical treatments generally are one of three classes:
- Topical Minoxidil
- Regenerative Treatments – ECM, PRP, and LLLT
- Medicines affecting the male hormone pathway
Minoxidil, a vasodilator, is FDA approved to treat hair loss. Testing showed that a 5% solution or foam applied to the scalp twice a day resulted in an increase in hair regrowth in 45 percent of the female subjects.
Regenerative Treatments:
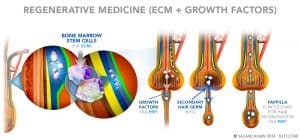
Extra Cellular Matrix (ECM), injected into the scalp, forms a structural scaffolding and signals the bone marrow stem cells to move to the scaffold area. The scaffold act as a glue that holds the stem cells in the scalp and helps them start to work regenerating the follicles and new blood vessels, collagen, fat cells and skin cells. The process may help the weaker hair cells become stronger and restore the normal hair growth cycle.
Platelet Rich Plasma (PRP) is prepared by putting a patient’s own blood in a centrifuge to concentrate and isolate the platelets and plasma from other blood cells. The concentrated platelets are activated, and they release growth factors. The fibrinogen in the plasma is also activated to provide the scaffold for growth factors to work and help the dormant papilla regenerate the hair. Platelet growth factors may reverse the miniaturization process and restore the normal hair cycle.
ECM and PRP can be injected into the scalp together; they complement each other in helping the weaker hair become stronger.
Low Level Light Therapy (LLLT) applies a lower dose of near infrared light to promote tissue regeneration and reduce inflammation. The existence of nearly all life on Earth is fueled by light from the sun; the sunlight spectrum ranges mainly from ultraviolet to visible and infrared light. LLLT is in the near infrared spectrum, from 600 to 1000 nanometers. Typically, it is applied for a few minutes on alternate days. LLLT may reverse the hair thinning and restore the normal hair growth cycle.
Medicine affecting the male hormone pathways can help stop hair loss in women. Many of these medications are indicated for other conditions but have been found to be helpful in off-label use for hair loss:
Spironolactone/Aldactone, is used to treat hypertension (high blood pressure) and edema (swelling). Spironolactone is an anti-androgen that works in two ways: it slows down the production of androgens in the adrenal glands and ovaries; and it blocks the action of androgens, in part by preventing dihydrotestosterone DHT from binding to its andogenic receptor, which is one of the major cause of hair loss.
Cimetidine/Tagamet mainly is used to treat gastro-intestinal ulcers. Cimetidine also has a powerful anti-androgenic effect and has been shown to block DHT from binding to the androgen receptor sites, which causes the hair loss.
Ketoconazole/Nizoral has antiandrogenic effects and can cause a reduction in the production of testosterone and other androgens by the adrenal gland and by the ovaries. Because of this action, it can be used to help treat hair loss.
Finasteride, taken as a 1 mg daily tablet, reduces the production of DHT and DHT-induced hair damage. Finasteride can reverse the miniaturization process, reducing the hair loss. The thin, weakened hair can revert to healthy, normal hair, especially in the crown area.
Cyproterone Acetate blocks the binding of DHT to its receptors. Because of its possible toxicity and potential long-term side effects, it is thought of as one of the last resorts for treating female hair loss.
Low-androgen-index birth-control pills decrease the production of ovarian androgens. They can also be used to treat genetic hair loss in women.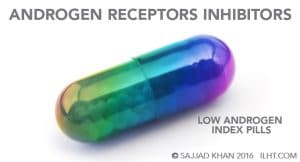
Cyproterone Acetate With Ethinyloestradiol/Diane 35/Diane 50, a contraceptive tablet, works by blocking some of the actions of those male hormones commonly present in women.
Surgical Treatments
Surgical treatments for hair loss include different types of hair transplant procedures. Hair transplant is the only proven way to restore hair permanently onto the bald or thinning areas of the scalp.
Under local anesthesia, hair is relocated from the back of the scalp to the thinning or bald areas. Because the transplanted hairs are genetically different from the ones that were lost, they are resistant to hair loss and will continue to grow permanently.
Natural and permanent results of hair transplantation demand clinical expertise and as well as artistic creativity and ability on the part of the surgeon.
Surgeons generally use one of the two standardized hair restoration techniques or a new technique still being perfected:
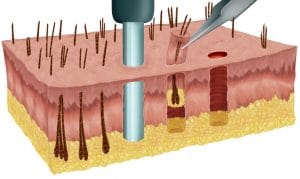
- Follicular Unit Extractions (FUE), in which follicular units are individually punched out from the back of the scalp and relocated to a thinning or bald area.
- Follicular Units Transplant (FUT), in which hair-bearing tissue is taken from the back of the scalp, individual follicular units are separated out from the tissue under microscopes, and the follicular units are transplanted into the thinning or bald area.
The technique of hair restoration surgery used on a particular client depends on her specific individual needs and lifestyle.
FUE
FUE requires the donor area to be partially or completely shaved, but most women do not want to shave the head completely. Even partially shaving the area results in lower hair volume in the donor area, which many women don’t like. Few women opt for partially shaving the area, especially because the FUE procedure already severely limits the number of follicular units that can be donated.
Special micro punches are used to remove the follicular units manually, motorized or robotically, then they are transplanted to the thinning areas. The goal is to have minimum damage during FUE.
Advantages Of FUE:
- Once the donor area heals, there is no noticeable scarring in the donor area.
Disadvantages Of FUE:
- An average 5% of the follicular units extracted are damaged.
- The surgery is noticeable for an average of 10 to 15 days.
- If the client likes to wear her hair long, it could take many months – even years – to get all the hair to grow back to the desired length.
FUT/Long Hair Technique
If the client would like to resume her usual routine the day following the surgery without it being noticeable, FUT is a good choice.
In FUT, an incision an average 0.5 mm deep is made at the upper and lower borders of the marked donor area. To extract the donor tissue, the incision margins are separated by special skin hooks without any further incision to avoid damage to the hair. The follicular units are then separated from the extracted tissue under microscopes.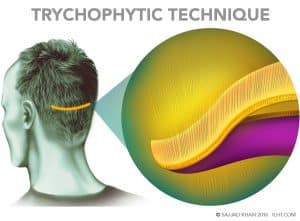
Removing that donor tissue leaves a 1 to 2 cm gap in the donor area, which is where the scarring can take place. However, the surgeon can reduce scarring by using the Trichophytic technique. The surgeon lays ECM in the tissue gap to promote healing, then shaves one edge of the gap and overlaps the edges to be fine-stitched together. As the incision heals, the hair will grow out through the fine scar line, which can make the scar undetectable even in short hair.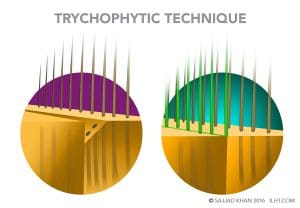 Advantages of FUT/Long Hair Technique:
Advantages of FUT/Long Hair Technique:
- Damage to less than 0.5 percent of follicular units during preparation for transplant, compared to as much as 5 percent in the FUE procedure.
- Higher follicular unit numbers transplanted and nearly 100% survival can help achieve the client’s goals in only one surgery.
- Long hairs transplanted in the hairline gives a good preview of the future hairline and outcome.
- Follicular units can be readjusted during the surgery if needed, depending on the initial look.
- There is no surgical downtime; the client could resume work the day after the procedure without it being noticeable.
Disadvantages of the Long Hair Technique:
- Stitches marks or a fine line scar in the donor area could be noticeable.
- The patient experiences temporary numbness in the donor and transplanted area.
- The client could see shock hair loss in the transplanted area (although hair lost due to shock grows back along the transplanted hair).
Reasons to Choose FUT
- There is no surgical downtime; the individual can resume work the very next day.
TREATMENTS FOR METABOLIC HAIR LOSS IN WOMEN
The doctor should regard nutritional deficiencies as the most likely cause for short-term hair loss and so carefully check for them. Micronutrient diagnostic tests detect deficiencies in essential hair nutrients such as water; protein; iron; Vitamins A, C, D and E; zinc; silica; selenium; copper; magnesium; potassium; calcium; omega-3 fatty acids; and B-complex vitamins, especially biotin, niacin and cobalamin. Once the deficient nutrients are added in the diet, the lost hair should grow back.
Iron Deficiency Anemia is treated by replenishing the body’s iron stores through eating food rich in iron and taking medicine or supplements.
Foods that will help increase the body’s intake of iron:
- Meat
- Poultry
- Fish
- Leafy greens
- Legumes
- Whole grains
Most people with an iron deficiency need 150 to 200 mg per day of elementary iron (2 to 5 mg of iron per kilogram or 1 to 1.5 mg per pound of body weight). Vitamin C (ascorbic acid) improves iron absorption, and some doctors recommend that individuals suffering from iron deficiency take 250 mg of Vitamin C along with the iron.
Lost hair due to dramatic weight loss will grow back once further weight loss is halted and the woman resumes a good nutrition and exercise plan. Usually, no medical intervention is needed.
Traction hair loss can be stopped by stopping the regular use of hair extensions and not pulling the hair back too tightly in braids or other close-to-the-scalp styles. Once the traction stress is taken away, hair usually grows back.
If hair loss is attributed to the use of a prescription medication, the woman should discuss with the doctor whether other medications for the condition can be used instead. Most of the time, once a prescription is substituted, the hair loss stops and the lost hair grows back.
Chemotherapy drugs often cannot be substituted, however. A cold pack applied to the scalp during chemotherapy can protect most of the scalp hair from the loss.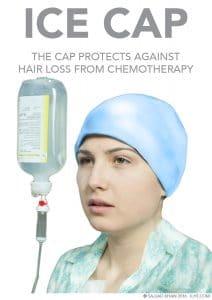
If hair loss happens in response to hormonal contraceptives, ask your doctor about using low-androgen-index contraceptives. If hair loss persists even with low-androgen-index contraceptives, consider non-hormonal means of birth control.
The standard treatment for hypothyroidism involves the daily use of the synthetic thyroid hormone levothyroxine. The patient is started on 50 micrograms, which can be increased, according to need, to 100. This oral medication restores adequate hormone levels, reversing the signs and symptoms of hypothyroidism and mostly reverses the hair loss.
Treatment of Hair Loss Due to Hyperthyroidism
Anti-thyroid medications and radioactive iodine are also used to slow the production of thyroid hormones. Sometimes, treatment of hyperthyroidism involves surgery to remove all or part of the thyroid gland. Restoring the normal hormones level mostly reverses the hair loss.
Treatment for Stress-Related Hair Loss
The following methods are effective in reducing the stress and stress-related hair loss
- Exercise to reduce the stress hormone cortisol
- Meditation can help desensitize stressful triggers
- Relax on weekends
- Create predictability at work and at home
- Eat healthy, complex carbs, oats, and whole grains to increase serotonin, a calming brain chemical
- Eat green, leafy vegetables: they provide magnesium, reducing the effects of stress
- The Vitamin C from citrus fruit will increase immunity and reduce stress hormones
- Nuts, especially almonds and pistachios, provide Vitamins E and B and healthy fat and help protect you against the effects of stress
- Fatty fish provides omega-3, which prevents a surge in stress hormones
- Avocado and bananas provide potassium and help reduce the increased blood pressure, which is a consequence of stress
- A complex carb snack at bedtime increases the brain-calming chemical serotonin and leads to better sleep
- Black tea blocks the formation of stress hormones after a stressful event
- Eating raw vegetables helps release a clenched jaw caused by stress
Pregnancy-related hair loss usually peaks three to four months after delivery. The good news is that this hair loss is temporary, and your hair should return to normal within six to twelve months. Pregnancy itself won’t cause harm to your hair, but nutritional deficiencies during pregnancy can, so if that is your issue, be sure to supplement your diet from food sources rich in B-complex vitamins, Vitamin C, Vitamin E, and zinc.
To reverse hair loss due to polycystic ovarian syndrome, the doctor may recommend combination birth-control pills—pills that contain both estrogen and progestin. These birth-control pills decrease androgen production, give the patient’s body a break from the effects of continuous increased androgen and increased estrogen which comes from androgen conversion into estrogen. Another medication, spironolactone, also blocks the androgen effect and reverses the hair loss.
Once a person recovers from extreme sickness or major surgery and resumes good nutrition and exercise plan, any lost hair usually grows back.
Women who have hair loss associated with menopause benefit from estrogen therapy, already considered the most effective treatment option for relieving all kinds of menopausal symptoms. Bringing the estrogen-androgen balance to pre-menopausal levels relieves menopausal symptoms, decreases the risk factors for heart disease, and reduces hair loss.